The Biden administration has issued guidance that states certain people may be “high-risk” and will more easily qualify for monoclonal antibody treatment and oral antivirals to treat COVID-19. This guidance is based on “race or ethnicity.”
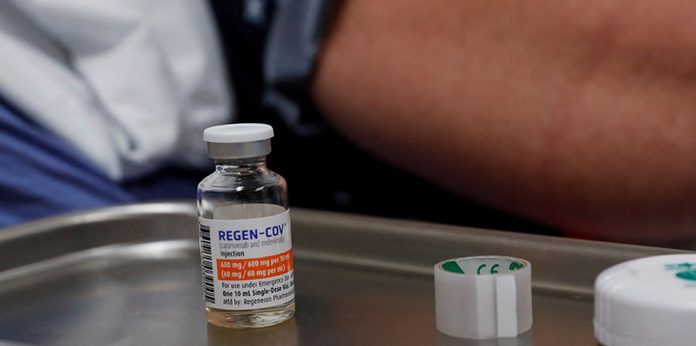
The Food and Drug Administration issued a fact sheet to healthcare providers approving emergency use authorizations for sotrovimab. This monoclonal antibody was proven to be effective against the Omicron variant. It is only approved for patients who are considered to be at “high risk.”
Updated December 20,21, the guidance states that “medical conditions or factors” such as “race” or “ethnicity” can “place individual patients at risk for severe COVID-19 progression.”
The FDA considers “high-risk” individuals to include those with multiple medical conditions such as obesity, diabetes, chronic kidney disease, diabetes, and pregnancy.
New York, Utah, and other states have made it clear that they will prioritize certain racial minorities over high-risk patients when it is time to distribute COVID treatments. The New York Department of Health published last week a document that detailed its plans to distribute monoclonal antibodies treatment and antiviral medications.
The plan contains a section about eligibility for the rare antiviral drugs that people need to be treated. It also includes a line that states that a person must have “a medical condition” or other factors that could increase their chances of severe illness.
A race or ethnicity that’s not White is a “risk factor,” as it is a result of “longstanding systemic inequalities and health problems.”
The memo states that non-white races and Hispanic/Latino ethnicities should be considered risk factors because they pose a greater risk of serious illness and death due to COVID-19. Utah’s guidelines for monoclonal antibody distribution in Utah state provide 2 points to residents who are “nonwhite” or “Hispanic/Latinx.” This is when they calculate their “COVID-19 Risk Score”.
“Race/ethnicity remains a risk factor in severe COVID-19 disorder, and the Utah COVID Score is one approach for equitable access to hard-hit communities,” the Utah guidance stated. It also reminded that the FDA’s national guidance “specifically states race and ethnicity may not be considered when identifying patients who are most likely to benefit from this life-saving treatment.”
The framework by the State of Minnesota also advises health care providers and clinicians to “consider the increased risk of progression of severe COVID-19 associated race and ethnicity when determining eligibility for the allocation of monoclonal antibodies therapies.”
The framework states that “FDA’s acknowledgment means that race, ethnicity, and other underlying conditions may be considered when determining eligibility for MAbs.” “It is ethically acceptable to consider race or ethnicity in determining eligibility for mAbs when data shows an elevated risk of poor COVID-19 outcomes (BIPOC populations). This risk cannot be adequately addressed if eligibility is based on underlying medical conditions (perhaps because of underdiagnosis of conditions that increase the risk of poor COVID-19 outcomes in these populations).